October is SIDS awareness month and was created to raise awareness about SIDS, understand how to reduce the risk of SIDS, and to promote safe infant sleep to prevent accidental sleep deaths in babies and toddlers. While a lot is unknown about the cause of SIDS (it almost always follows a period of sleep), just by following safe sleep practices, there has been an overall drop in SIDS related deaths.
Thankfully the AAP has developed a very easy way to remember the safe sleep rules for your little ones! Learn about the Triple Risk Model, the ABC’s of safe sleep, other important ways to reduce the risk of SIDS, things to consider while pregnant and postpartum, and why all of this is so important, including the most recent research!
1. Learn about the triple risk model
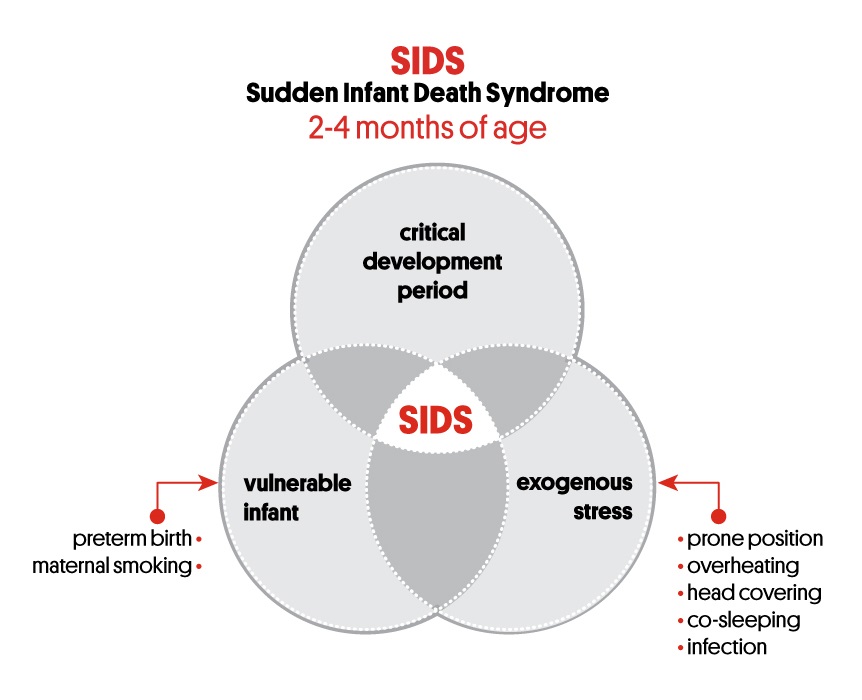
Before we explore the ABC’s of safe sleep, it’s important to understand the “triple risk model” which is how the risk factors for SIDS interact and may lead to an infant dying suddenly and unexpectedly.
The Triple Risk Model poses that
- a vulnerable baby
- at a critical period in development,
- when exposed to an external stressor with which they are unable to cope may die from SIDS.
The first factor in the triple risk model is a vulnerable baby. This is an infant who appears healthy but has an underlying abnormality or weakness which may only become apparent when they are exposed to stress. This abnormality could be genetic, defects with their heart or lungs, or issues with their arousal mechanisms.
The second factor is during a critical period in development, particularly the first six months of life. Babies are growing rapidly and it may be that their changing bodies destabilise their internal systems, especially if they have an underlying weakness or vulnerability.
The third factor is external stress (or outside/environmental challenges). This would include sleeping on their stomach, sleeping on a soft surface, putting the baby in a position where their chin rests on their chest, bedsharing, or an upper respiratory infection.
Per Red Nose, “No one risk factor in isolation is likely to be sufficient to cause death, and provided the infant survives the first year of life, may no longer be of any significance. However, when a vulnerable or compromised infant is confronted with one or more stressful situations, several of which are now clearly identified as risk factors, and from which the majority of infants normally escape, the combination may prove fatal.”
https://rednose.org.au/article/the-triple-risk-model
2. Learn about the ABC’s of safe sleep
The AAP has determined through years of research that the safest place for your baby is:
A- Alone
B- on their Back
C- in their Crib (or safe sleep approved bassinet or pack-n-play)
A- Alone
Alone means without anything else in their sleep space including bumpers (yes, even mesh ones), stuffed animals, blankets, sheets, pillows, and loveys. While all of that is cute when decorating a nursery, it is not practical and it is best to stick with a tight fitted sheet, with a swaddle or Kyte BABY sleep bag!
Mesh bumpers still pose a strangulation risk and also serve as a means for helping an older infant/toddler climb out of the crib resulting in injury. We want to keep our little ones in their safe sleep space for as long as possible!
A good rule of thumb is that anything that attaches to the crib is unsafe to use as they risk entrapment, suffocation, or strangulation. According to a study in the journal Pediatrics, “the number of babies who died because of bumpers tripled in the last seven years of data available. From 1983 to 2012, bumpers may have been involved in 77 deaths.”
Just remember, no deaths have been associated with getting a limb stuck between the crib slats. If you feel like your baby is getting a leb stuck often and it is interrupting their sleep, then a Kyte BABY sleep bag is a great solution for those busy little babies!
B- Back
The “Back to Sleep” campaign was launched in the 90’s as part of the safe sleep campaign when SIDS deaths were on the rise. It significantly lowered the rate of SIDS death from then on. Therefore, it is important to always place your infant on their back to sleep for the first 12 months.
Once your baby can roll, they are safe to sleep on their belly should they choose that as their position of comfort. Thus, if they roll in their crib, it’s completely fine to leave them that way (so long as your sleep space is free of any loose objects). If you were to put your infant in a position they can not easily get into, they could get stuck in a way that blocks their airway.
A study out of Australia actually found that babies who sleep on their belly have lower levels of oxygen in their brain than babies who sleep on their back.
Swaddling should be discontinued once an infant is rolling, however a sleep bag is completely safe to use when they are more mobile. A Kyte BABY sleep bag will keep their arms free and aid in getting into or out of different positions while keeping them warm and safe.
But what about babies who have reflux, should you be concerned about choking? From Kids Health, “Many parents fear that babies put to sleep on their backs could choke on spit-up or vomit. However, only babies with certain uncommon upper airway malformations may need to sleep on their stomachs. There's no increased risk of choking for healthy infants and most infants with gastroesophageal reflux (GER) who sleep on their backs.”
This is definitely a conversation you should have with your physician if you are concerned, regarding the safest position for your baby to sleep in.
C- Crib
A crib with a firm sleep surface and tight, fitted sheet that meets the safety standards of the Consumer Product Safety Commision (CPSC) is the safest surface for your little one to sleep on. You might think they need something softer, but when you place your baby down alone, on their back, in their crib on a firm surface then the mattress should not indent at all (see below).

Most crib mattresses will come with an infant and a toddler side so double check that you have the correct side up in your little one’s crib. Only use the toddler side when they are at the age recommended by the manufacturer.
A mattress that is too soft or indents when you place them on it can make it difficult to get in and out of positions if they needed and can cause positional asphyxiation (where their airway is blocked due to their chin resting on their chest). You will want to stay away from mattresses with memory foam and you don’t have to succumb to marketing terms like “breathable” or “reduces/prevents the risk of SIDS.”
As long as they are approved by the CPSC, there is nothing to prove one mattress is better than another! Some crib mattresses may not fit in every crib so make sure the dimensions are right for your specific crib and that there are no gaps around the mattress that could cause entrapment.
Per the AAP: "There is no evidence that special crib mattresses and sleep surfaces that claim to reduce the chance of rebreathing carbon dioxide when the infant is in the prone position reduce the risk of SIDS."
It’s important to avoid putting your baby down to sleep on a surface like a couch, chair, or your own bed as these are likely too soft and have pillows or blankets around. The car seat is also not a safe space for sleeping outside of the car so it’s best to move them to a firm mattress when you get back home!
3. Other important ways to reduce the risk of SIDS
Room share for the first 6-12 months of your baby’s life. Room sharing is simply sharing your room with the baby- it is not the same as sharing a bed with your baby. Your baby should still have their own separate sleep surface such as a crib or bassinet.
In bed sleepers have not been evaluated by the AAP so they can not attest to their safety or recommend them at this time. Attaching the crib to the bed has also not been approved as safe use as it can lead to entrapment.
Introduce the pacifier once you’re comfortable doing so. There is no evidence to support “nipple confusion”, however it is best to wait for feeding to be established and make sure baby is gaining weight to avoid missing baby’s hunger cues.
It is okay for a pacifier (without a stuffed animal attached to it) to be in the crib with your baby if it falls out while they are sleeping. If your baby does not love the pacifier, you do not have to force it! You can always offer it here and there to see if your baby begins to accept and love the pacifier.
Keep the room at a comfortable temperature. Overheating is a risk factor for SIDS so try to keep the thermostat between 68-72 degrees or layer appropriately with a sleep bag instead of a blanket.
| “This made a huge difference in my son’s sleep routine! As soon as we zip it up, he starts getting snuggly and tries to lay his head down. So soft and keeps him warm without letting him overheat. I will be buying another!” -Amber Roberts |
Make sure you check that you are using the appropriate TOG for your nursery temperature or that you are using the appropriate layers with your TOG. Read these helpful blogs to determine the right one for your little one!
Practice a lot of tummy time during supervised awake time! This is important for strengthening their muscles and develop their motor skills for rolling so that they can get out of an unsafe situation. Once they can roll on their own, a baby is safe to sleep in whatever position they find comfortable because they have demonstrated they have enough strength to move out of any compromising position so long as their sleep space is empty of any loose objects.
4. Things to consider while pregnant and postpartum
Do not smoke while pregnant or any time around your baby. It’s important to not expose them to second-hand smoke even if you’re outside! Keep your car and home smoke free.
Do not use illicit drugs, an excessive amount of alcohol, or drugs that inhibit your response time and keep you from waking as easily.
Breastfeed if possible as it helps to reduce the risk of SIDS. Even a little bit is better than none!
5. But what about bedsharing?
The AAP acknowledges that bedsharing occurs for the majority of families, especially if you are breastfeeding. They suggest only bringing your baby into your bed for play, feeding, or comfort and returning them to their safe sleep space when they’re done eating and ready for sleep.
If there’s a chance that you’ll fall asleep, then make sure there are no pillows, sheets, blankets, or any other items that could cover your baby's face, head, and neck, or overheat your baby. The AAP suggests moving the baby to their separate sleep space as soon as you wake up.
This is not to say that you can never hold your baby to sleep! “An awake adult holding a sleeping baby on their chest should be OK, although the preferred position for sleep is supine” (lying on the back), Feldman-Winter says. “If this is more than a quick nap, the infant should be placed supine in a crib, Pack 'n Play, or other safe surface.”
6. So why is this important?
SIDS is still one of the leading causes of deaths in babies under 1 year of age and ~90% of SIDS deaths occur in babies under 6 months of age. (This diagnosis should only be given after a thorough postmortem investigation and death scene investigation including baby’s environment while sleeping). It’s a diagnosis of exclusion.
Boston Children’s Hospital says, “SIDS is part of a larger category of unexpected (as opposed to unexplained) infant deaths called SUDI (sudden unexpected death in infancy). Babies who die suddenly but whose causes of death are later explained (infection, brain abnormality, cardiac dysfunction, etc.) also fall into this SUDI category.”
According to the AAP, “Research showed that between 1993 and 2010 the percent of infants placed to sleep on their backs increased from 17% to 73%. Following the initiation of the “Back-to-Sleep” campaign, the number of infants dying from SIDS has decreased to 2,063 per year as of 2010.”
The most recent data is from 2017 from the CDC (via the chart below) and states that “1,400 deaths were due to SIDS, about 1,300 deaths due to unknown causes, and about 900 deaths due to accidental suffocation and strangulation in bed.” Check out this blog to read more about SIDS vs ASSB.

However, the next chart shows that while the rate of SIDS deaths has decreased, the rate of accidental deaths has risen. This could be due in large part to better reporting and categorizing of infant deaths instead of lumping all deaths as SIDS. According to WebMD, The number of babies dying from accidental suffocation and strangulation in bed skyrocketed 184% from 1999 to 2015.

Medical experts have not found a cause, however there are certain factors that may play a part in contributing to SIDS such as:
- Physical factors (brain abnormalities, low birth weight, respiratory issues)
- Sleep environment (tummy sleepers, soft bedding/loose blankets, bedsharing)
- Other factors (boys more than girls, more vulnerable in months two-four, exposure to cigarette smoke, and a family history)
While babies outgrow being at risk of SIDS, it is still important to be mindful of sudden and unexplained death in childhood (SUDC). This is a category of death in children between ages one to eighteen that is unexplained after a thorough investigation, including an autopsy.
At this time, there is no way to predict it or prevent it; a seemingly healthy child goes to sleep and doesn’t wake up. It is labeled a SUDC death when they can find no other known cause. Unfortunately, there is no way to even know how often SUDC occurs because the World Health Organization lacks a way to record sudden and unexpected deaths in childhood. It still remains a statistically lower instance than SIDS.
Although there is no way to prevent SUDC, it’s still important to consider safe sleep for toddlers.
- Make sure your child’s crib is away from any objects with cords including window blinds.
- Be mindful of items your child may be able to reach and pull into their crib with them.
- There is still no need for a pillow or blanket at this age as suffocation and strangulation can still occur.
- If you do use a pillow, make sure your child is over the age of two. We have sleep bags that will get your child well through toddler-hood so there’s no need for a blanket!
- A bare crib is still the safest option, even if your child is over the age of one.
While SIDS cannot be prevented, there are definitely steps you can take to reduce the risk, but even parents who follow all the safe sleep rules can lose a child to SIDS. Awareness of safe sleep recommendations has increased, but not all parents understand why the recommendations are so important, especially when their family or friends has survival bias (“I put my baby to sleep on their belly and they lived!”).
Despite years of research, there is still no known cause of SIDS. Many theories have been explored, but nothing consistent has been identified.
New research released in 2019 says there may be a link between sudden, unexpected and unexplained deaths and malfunctioning serotonin receptors in the brain. These receptors function as a “suffocation alarm” and ensure that blood oxygen and carbon dioxide levels are healthy.
But according to an opinion review by Gordon Buchanan, a neurologist and epileptologist at the University of Iowa, there’s “a rare neurological difference causes some people’s brains to be bad at detecting when blood CO2 levels get too high — which is a signal to our bodies that we could be suffocating. Instead of waking up like most people would, those with this defect stay asleep and are seemingly powerless against what’s happening to them.”
Furthermore, a team of researchers found a genetic mutation affecting respiratory muscle function was associated with a subset of SIDS cases.
Boston Children’s hospital is finding that the brainstems of SIDS infants have lower levels of the serotonin and a specific protein to signal alertness. They also had significantly fewer receptors for serotonin and another neurochemical in the brain. These abnormalities are thought to prevent SIDS infants from properly controlling the vital functions that keep them alive and ultimately to lead to their death.
Dr Kinney and colleagues are currently working towards a means of identifying those infants who are at increased risk of SIDS, with the ultimate goal of developing a treatment that will protect them from SIDS.
Since there is no end-all, be-all advice to prevent SIDS yet, the best thing you can do is follow the safe sleep advice in reducing the risk as much as possible.
Remember your ABC’s of safe sleep, other things to reduce the risk such as room sharing, introducing the pacifier, keeping the room at a comfortable temperature, not letting baby get overheated, a lot of supervised tummy time, staying away from second-hand smoke, breastfeed if possible, and do not use any illicit drugs or abuse alcohol.